Transplantation medicine continues to be an evolving field, with much still to understand.
Mere decades ago, patients and donor organs were matched by little more than ABO blood type. Today, Bloodworks’ Human Leukocyte Antigen (HLA) lab runs thousands of tests every year to ensure that patients in need of solid organ transplants (heart, lungs, liver, kidney, etc.) receive the right organ from the right donor.
ABO blood groups and Human Leukocyte Antigen (HLA) are components of the immune system that we think about often at Bloodworks. But they aren’t the body’s only antigenic targets: neutralizing responses to molecules like proteins, sugars, lipids, and other markers found on viruses, bacteria, pollen, or any other cells that don’t specifically belong to you.
What is HLA? Learn more on Bloodworks 101:
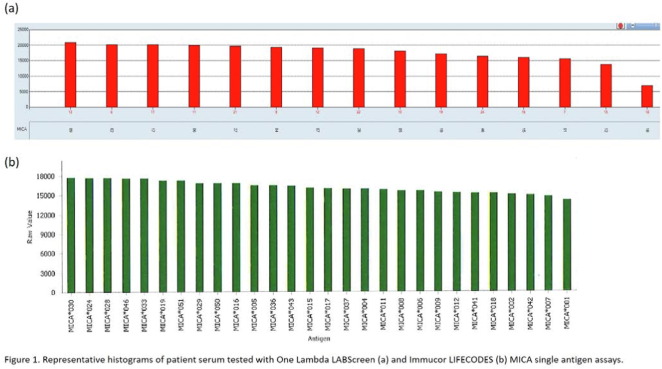
The Major Histocompatibility Complex class I chain-related molecule A (MICA) is another form of antigenic target. Currently, it is not common practice to screen for MICA antibodies when testing for organ compatibility.
However, work done by our HLA lab suggests that maybe we should.
Bloodworks recently looked into the case of a young double-transplant patient whose donor heart seemed like a good HLA match. However, their body was still rejecting the organ.
We determined that this patient had a developed a MICA antibody, which likely contributed to rejection.
This case study highlights a potential association with MICA in poor transplant outcome and the role MICA plays in transplant success and suggests that it may prove useful to test for MICA along with HLA (and potentially other markers) in the future.
GSTT1 is an enzyme found in liver, kidney, and red blood cells that helps neutralize toxins. However, anywhere from 10-50% of the population has a genetic mutation that makes them susceptible of creating antibodies against GSTT1.
Kidney and liver transplant patients who have this mutation may experience higher rates of antibody-mediated rejection (AMR): graft complications resulting from antibodies.
Bloodworks HLA lab found that GSTT1 antibodies are present in association with AMR in patients with this mutation but that the antibodies themselves do not appear to lead to the increased graft problems. Therefore, what seems to be happening is that anti-GSTT1 antibodies respond better to rejection treatment that other non-HLA antibodies.
Although the patient is going through rejection, these antibodies predict a better outcome.
To advance our understanding of non-HLA antibodies in organ transplantation, we need to be able to reliably identify and measure antibody response. We need the right tools.
There are two commercially available non-HLA assays (tests). One test looks at 39 different antigens (“beads”) and the other looks at 60, with 25 antigens in common.
Until recently, however, there hasn’t been a lot known about how to interpret the results or how comparable the two tests even are.
So, our HLA lab decided to find out.
Bloodworks collected serum from 62 living kidney donor candidates and focused on the 25 overlapping tests.
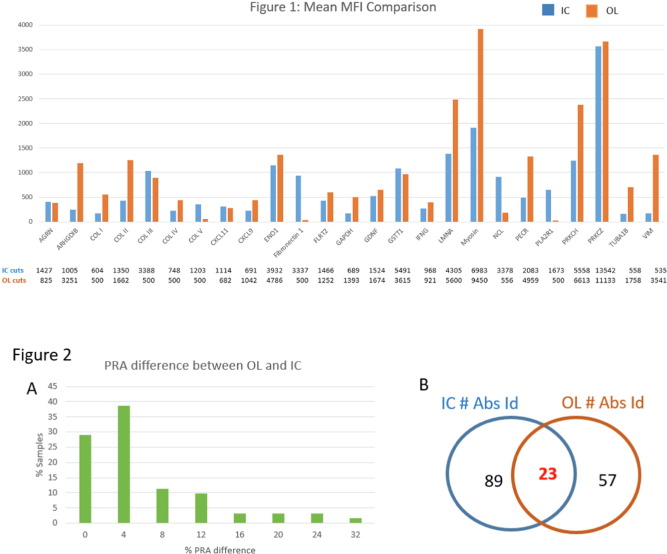
The results imply that there’s enough variability between the tests that more studies are needed to clarify the differences.
It may not be a conclusive answer, but we’re one step closer to improving outcomes for transplant patients locally and around the world.
Tell Us What You Think!